MBST® is designed to stimulate cartilage cells to regenerate, helping to relieve pain, improve mobility, and support active living with an improved quality of life.

75% of working people experience occasional or chronic back pain. It is the second most common reason for sick leave¹ and often leads to extended periods of absence. Persistent back issues may even result in early retirement.
Those living with chronic pain know how much it can impact their quality of life, affecting not only leisure time but also daily routines and work.
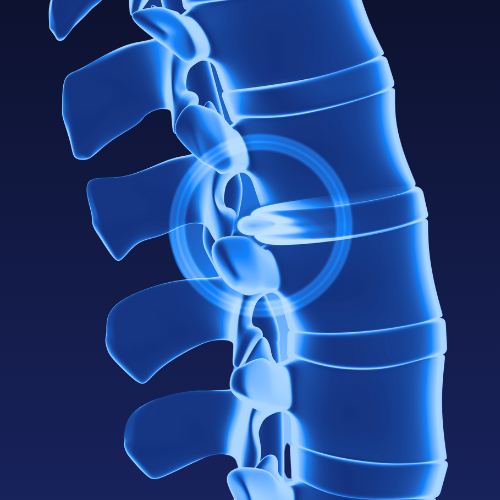
Knowing the cause of the pain is essential for a successful treatment. But back pain can have many causes: prolapsed disc, degenerative changes due to wear and tear, acute inflammation… Back pain can also be a symptom of other conditions, such as vertebral fractures caused by osteoporosis.
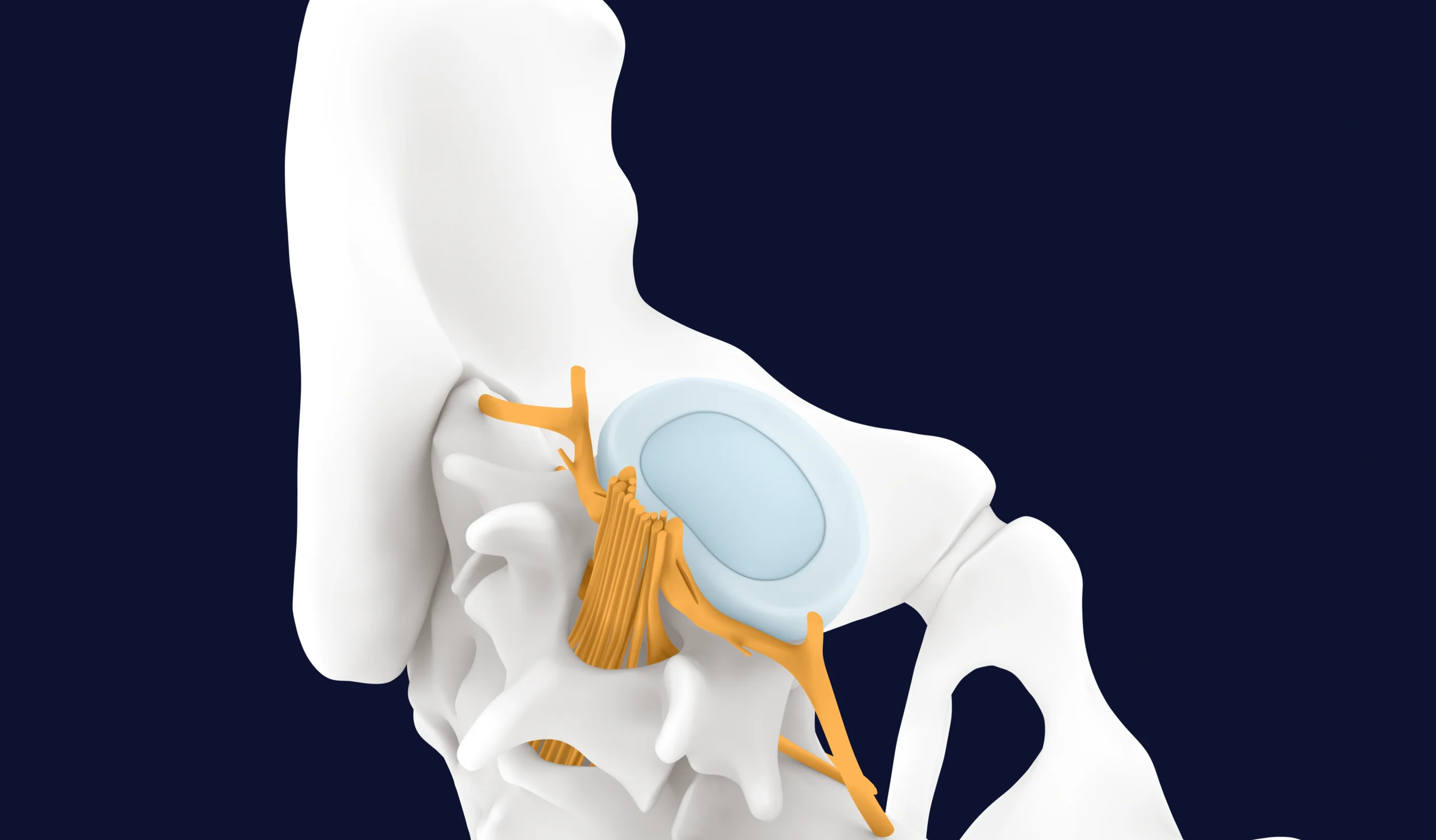
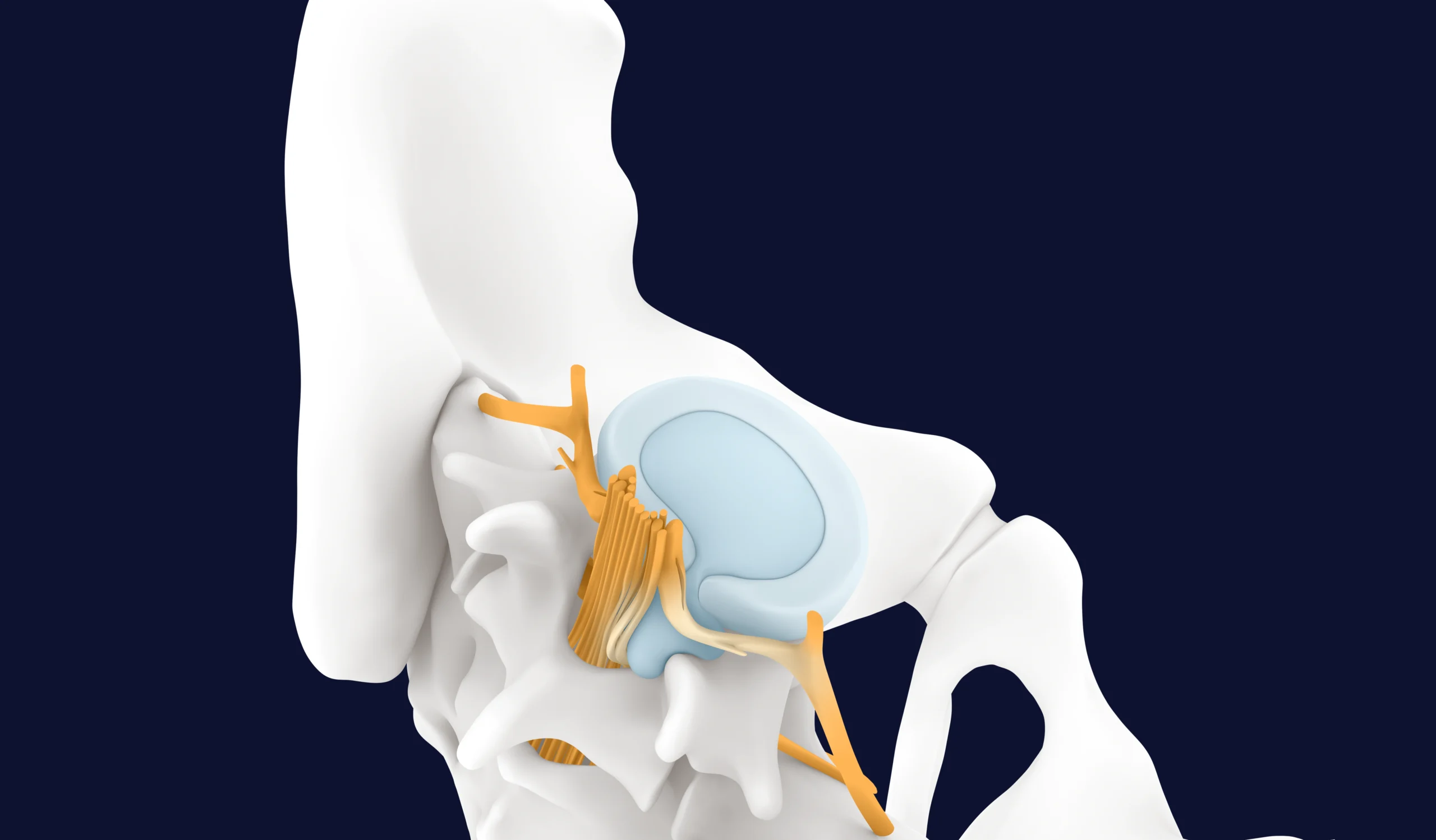
Intervertebral discs cushion the vertebrae, while facet joints allow the spine to move. This vertebral canal protects the nerves and the spinal cord. The surrounding muscles support the spine, working alongside intervertebral discs, bones, cartilage, nerves, and muscles. As a complex system, damage to one part of the spine often causes issues in other areas.
This is why a comprehensive treatment plan that combines different therapies is important—to quickly reduce pain and promote long-term recovery.
Most conventional treatments focus only on symptoms, using pain-relieving or anti-inflammatory drugs or muscle relaxants. Because disc tissue has a slow metabolism, the body’s natural regeneration takes a long time and often cannot keep up with the damage caused by wear and tear.
Failed treatments for chronic pain not only leave patients with ongoing pain and limitations but also create worries about future employment and financial security.
Many patients seek quick relief through surgery, but health insurance data has consistently shown that up to 88% of back surgeries are unnecessary.² Unless surgery is urgently needed, such as for paralysis, non-surgical treatments combined with physiotherapy are often more effective and less invasive.²

This may activate natural repair processes to promote regeneration and repair mechanisms. Quick pain relief can make everyday activities and effective physiotherapy much easier.
MBST® aims to support the body’s natural regeneration processes directly within the cells.
Targeted cell stimulation encourages various biophysical processes within the tissue, potentially promoting regeneration and tissue development.

Studies show reduced pain levels—sometimes even complete pain relief—along with improved mobility and movement.¹¹
“I would recommend the therapy to everyone! Since then, I have been pain-free and regained my mobility.”
Herniated disc and immobility of the left arm
“The cervical spine is freely movable and I can already play tennis again without any discomfort.”
Inflammation of the spine with damage to the intervertebral discs
“Without MBST®, I probably wouldn’t have been able to return to work so quickly.”
Herniated disc and immobility of the left leg
MBST® is a certified medical product used only in the medical field. It’s offered by practices, clinics, and centres as part of their treatment options to ensure you receive the best possible care for your condition.
The TÜV-certified manufacturing process ensures the quality, safety, and reliability of the MBST® therapy worldwide.

Patient data shows that significant pain reduction could still be observed years after therapy.* If needed, MBST® treatment can be repeated as often as required.
1 Gesundheitsreport DAK, 2024, dak.de/forschung-1282 | 2 Zweitmeinung Rücken-OPs | Die Techniker – Presse & Politik (tk.de) TK, 2024, Pressemitteilung | 3 Steinecker-Frohnwieser et al. 2014, J. Orthop. Rheum., 9/2014 | 4 Steinecker-Frohnwieser et al. 2018, Clin Exp Rheumatology 36, 294–301 | 5 Thöni et al. 2021, Chronobiology International, DOI: 10.1080/07420528.2021.1910288 | 6 Steinecker-Frohnwieser et al. 2021, Int J Molecular Sciences 22, 5959 | 7 Mann et al. 2022, frontiers in cellular neuroscience 16, 859545 | 8 Rad et al. 2024, Cells 13, 1544 | 9 Kullich et al., 2006, Journal of Back and Musculoskeletal Rehabilitation, 19, 2006, 79–87 | 10 Salomonowitz et al., 2011, Z Orthop Unfall, 2011, 149(5), 575–581, DOI: 10.1055/s-0031-1280121 | 11 Kullich et al. 2013, SCHMERZnachrichten 4a | 12 van Laack et al. 2011, Orthop Praxis 47, 11/2011, 536–543
You are currently viewing a placeholder content from Google Maps. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More Information